
PhotoXpress
Creative Minds: Making Sense of Stress and the Brain
Our ‘fight or flight’ impulse can do lasting damage.
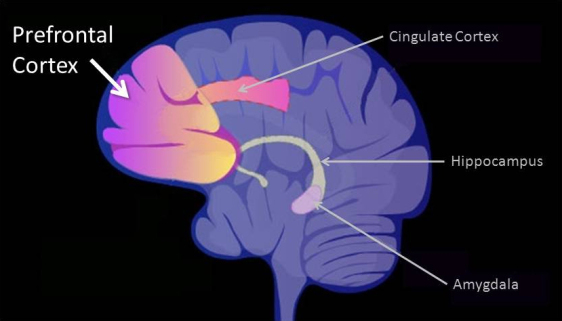
Right behind your forehead lies the most recently evolved region of the human brain: the prefrontal cortex, also called the PFC. It’s a major control center for abstract thinking, thought analysis, working memory, planning, decision-making, regulating emotions, and many of the things we most strongly associate with being human. But in times of stress, the PFC is literally taken offline, allowing more primitive parts of the brain to take over.
Amy Arnsten, a neuroscientist at the Yale School of Medicine, New Haven, Conn., has pioneered the study of stress on the brain and how impaired regulation of stress response in the PFC contributes to neurological disorders, such as attention deficit hyperactivity disorder, schizophrenia and Alzheimer’s disease. In these disorders, cells in the PFC are negatively affected, while those in the primary sensory cortex, a more primitive part of the brain that processes vision and sound, are thought to remain relatively unscathed. With support from a 2013 NIH Director’s Pioneer Award , Arnsten hopes to uncover why the PFC is more vulnerable to disease than the primary sensory cortex—and how we might be able to prevent or reverse damage to these circuits.
It might first help to understand why we have a brain that halts higher thinking functions when facing stress. Perhaps it doesn’t make much sense—until you think back to early humans. When our ancient ancestors encountered a deadly threat—like a saber-tooth tiger or blazing forest fire—they needed to make split-second decisions, not engage in thoughtful deliberations. Our primitive brain is wired to cause us to freeze, fight or take flight when facing danger. After the threat vanishes, the PFC goes back online and is reconnected.
In modern times, it seems that this primitive disconnect mechanism can sometimes hinder our ability to function well, allowing much milder stressors to short circuit our thinking. More importantly from the standpoint of medical research, it seems that the chemical pathways that enable this disconnect of the PFC may also make this region of the brain more vulnerable to certain diseases.
In fact, Arnsten has discovered that the junctions, or synapses, between neurons in the PFC can be rapidly weakened or strengthened depending on their chemical environment. When we are alert and feel safe, modest levels of arousal chemicals—like norepinephrine and acetylcholine—help PFC cells communicate efficiently, giving us the power to think, remember and plan. When we are under stress, however, very high levels of these same chemicals drive a vicious cycle inside the PFC cells, weakening synaptic connections and disrupting communications. If the stress continues for a long period of time, say for days or even weeks, the PFC actually loses the connections, although they can regrow if the stress goes away. (Note to fans of the recently announced BRAIN initiative, which aims to define a complete census of all cells in the human brain and determine how actual brain circuits work in real time: the broad, sweeping conclusions just cited here need to be contextualized by the recognition that the PFC is made up of a wide variety of different cell types with different functions.)
In healthy brains, an enzyme called PDE4A is strategically positioned near the synapse to halt the stress-driven cycle of chemicals, thereby allowing PFC cells to reconnect. Intriguingly, some people with schizophrenia have genetic variants that weaken PDE4A, as well as the molecule that anchors it. This may make them particularly vulnerable to thought disorders when they are stressed.
New data from Arnsten’s lab reveal that humans also lose PDE4A as they grow older. This can relax the normal checks on the stress cycle and weaken PFC connections, contributing to minor cognitive lapses, such as “Where are my reading glasses?” The loss of PDE4A also drives production of phosphorylated tau—a protein involved with the progression of Alzheimer’s and other neurodegenerative diseases. What’s more, head injuries can trigger the stress-driven cycle of chemicals in the PFC. This might explain why, although they share no obvious connections, head injury, emotional trauma and advancing age are all risk factors for developing Alzheimer’s disease.
Arnsten’s fascination with the neurological effects of stress dates back to her college years, when she spent a summer working at a New Jersey state psychiatric hospital. One patient was a middle-aged physicist who had schizophrenia. When this man discussed physics or astronomy, Arnsten found it almost impossible to tell that he suffered from schizophrenia. But one day, when they were chatting about some planetary phenomenon, a nurse mentioned the name of a doctor who was feared by many patients. The mere mention of this doctor’s name triggered a stress attack that caused the patient’s speech to disintegrate into what Arnsten describes as “word salad.” After about five minutes, the man calmed down and his remarks once again became coherent. That was Arnsten’s first inkling that stress could cause a dramatic disconnect in the brain.
Arnsten’s lab has already helped develop a drug to treat one particularly common disorder involving the PFC: ADHD. This nonstimulant drug, an extended-release form of guanfacine called Intuniv, is approved by the FDA for children ages 6 through 17 with ADHD. The drug mimics norepinephrine, one of the chemicals involved in the PFC stress cycle, thereby helping to strengthen the regulation of attention, impulses and emotions.
With Alzheimer’s disease and schizophrenia, which together affect nearly 8 million people in the United States, Arnsten has set her sights on a couple of the toughest challenges in biomedical research today. Her hope is that if she can find compounds that mimic the normal effects of PDE4A, it may be possible to slow or even prevent the devastating damage that these diseases inflict on the part of the brain that plays such a crucial role in making us who we are as humans.
Source: Brain Regions , National Institute of Mental Health, NIH
NEXT STORY: Generational Divide? What Generational Divide?







